Don's gem's
The Wizard's potion
These are some of Don's interesting comments from the Friday morning case conferences. Any errors in this section are solely the poor recording of otherwise accurate comments, due to the pressure of the quantity of interesting comments. This section is updated weekly.
To see the cases click here
This section has outgrown it's page and been subdivided. Previous sections are linked below.
| 2001 | July | August | September | October | November | December | ||||||
| 2002 | Jan | Feb | March | April | May | June | July | August | September | October | November | December |
This page last updated on 05/06/2003 09:56:57 PM
June 21st 2002
A la Michelle
1)
*Os trigonum syndome- un-united lateral tubercle of talus - fuses by 10 - 13 yrs
*Tethering of the FHL and laxity of the lateral ligaments may predispose to the syndrome.
*Sloping of the posterior malleolus may predispose to Os Trigonum syndrome - there is mention in some of the patients in the study presented that longer lengths of the slope may relate to the development of the Os trigonum syndrome).
*SER 4 - supination and external rotation - most common type of the Lauge-Hansen classification.
*Tib Fib ligs involved (not talofib and calcfib - which are involved in the fractures lower down).
*Some reports of Stage 2 moving straight to 4 but not of Stage 1 developing into Stage 3 without the intervening Stage 2).
*Lateral process of calcaneus with a fracture is associated with snow-boarding!!
2)
*Keinbocks - expect it in 20 - 40 yrs. The lunate is predisposed to Keinbocks due to the position of the lunate in the carpus, ulnar minus variance and also the blood supply.
It is a chronic stress-related problem, not as a discrete involvement of bone but then you have fragmentation in the bone later in the disease. 75% association with ulnar minus variance - therefore it is a known association. It is seen in ulnar neutral but rarely with the ulnar positive.
3)
*Plain-film - huge sub-acromial enthesophyte- it is associated with external or shoulder impingement syndrome. There was a large degree of proliferation around the glenoid of the GH joint. Look at the Museum of Man specimens and many of them exhibit a similar pattern- may be ossification of the labrum (although it is usual even in the distribution around the entire cirumference of the glenoid) or enthesophytes of the capsule.
4)
*Rice bodies - synovial proliferation is not specific for disease and you have to consider the age of the patient and also how you would expect the plain-film to appear. Also here the question is also is it related to the previous injury.
*Brucellosis is apparently common in the North of Portugal.
*TB may have to be diagnosed with a synovial biopsy, not necessarily from a synovial tap.
5)
*Posteromedial cysts about the knee are more common in the lateral portion of the joint.
6)
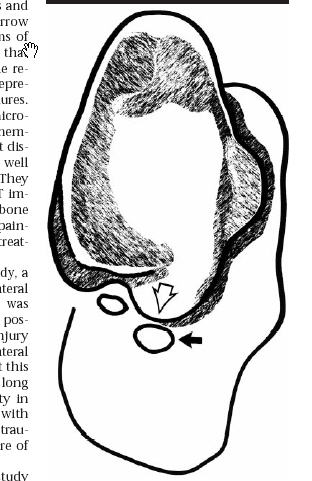
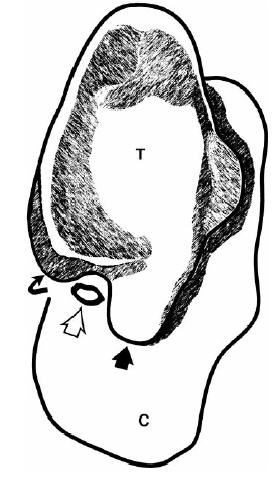
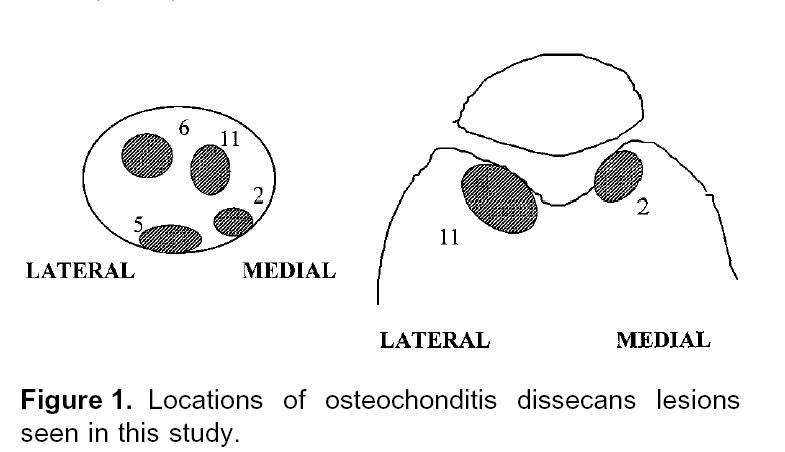
*Dorsal defect of the patella - here is an osteochondral defect in a 15 yr old male. Osteochondritis dissecans of the patella - quite unusual. Usually at least competitive if not professional athletes, with signs and symptoms including peripatellar pain and "insecurity" of the knee, although one case in the report quoted no pain in this area was present. Location seems to be variable, most common in the study presented in the supero-medial region of the patella and along the lateral portion of the trochlea.
*Dons rule!!!! Divide patella with a transverse line in the mid portion - then osteochondritis dissecans should lie inferior to this - Dons rule to separate from the dorsal defect of the patella but this does not seem to be the case now.
a)
*Gout - 8.4 per 1000 persons, 40% are familial.
Hyperuricicemia - related to the uricase gene, which assists in the metabolism of uric acid and in humans it is switched off - hyperuricemia may protect against degenerative diseases like RA.
*RAGU - is not a spaghetti sauce but the combination of RA and Gout - seeing partially calcified tophi and then in other places looking like RA.
*CPPD and Gout are related and favours fibrocartilage.
*Finding proliferative bony changes on a lateral plain film of the mid-foot is suggestive though not pathognmonic of Gout - it should at least make you think about it.
b)
*Tear of the Extensor Carpi Ulnaris - most common tear.
*Remember the Caput Ulnae syndrome associated with RA.
c)
*Hyperextension lateral view for bringing out the vacuum in degenerative disc disease. *Extensive sclerosis - based about the disc mainly. Terms like discogenic or hemispherical sclerosis are perhaps misleading.
d)
*Posterior Ankle Impingement - Repetitive or acute forced plantar flexion of the foot. Abnormal signal in Os Trigonum or the lateral tibial tubercle.
e)
*Diabetic foot - Look for osteomyelitis, cellulitis, osteolysis, neuropathic arthropathy, osteopenia and arteriosclerosis.
f)
*Abnormal high signal in Hoffas fat pad - superolateral impingement syndrome - high signal on fluid sensitive sequences in superolateral aspect of Hoffas fat pad.
*Q - angle - a measure of where the patella sits with respect to the femur and tibia - a long axis line running through the patella and tibial tuberosity and then the patella and long axis of the femur and then one looks at the position of the patella and the angle.
g)
*PCL abnormal density in the plain film. Associate chondrocalcinosis and PCL crystal disease.
May 24th 2002 Ortho
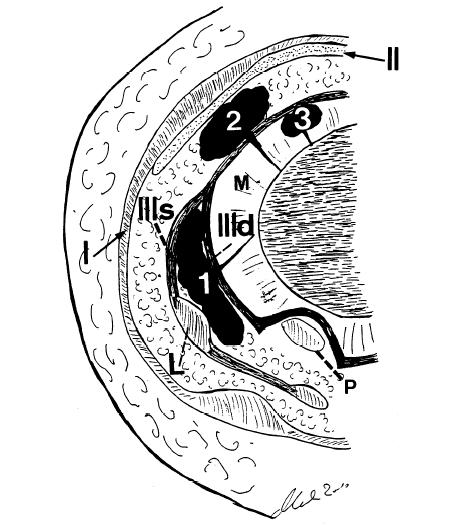
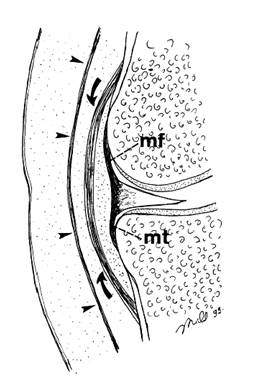
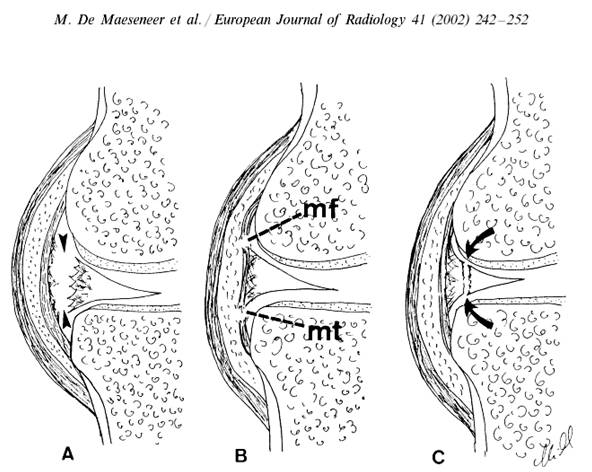
1.Meniscocapsular seperation is usually posteromedial.
![]()
A: Corner tear
B: Meniscal displacement
C: Peripheral edema, irregularity
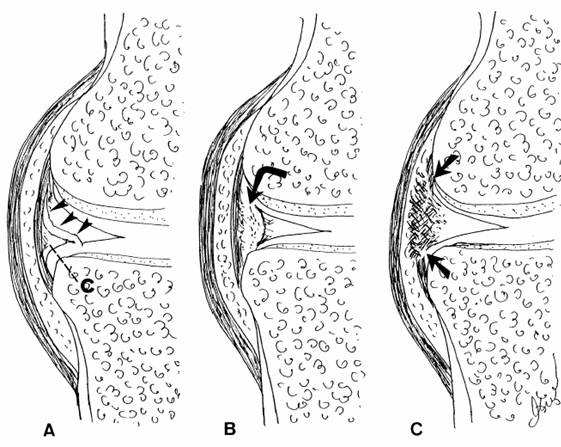
A: Corner tear B: Meniscal displacement C: Peripheral edema, irregularity
MR signs of meniscocapsular seperation.
Fluid deep to MCL
Increased perimeniscal signal intensity
Abnormal lateral fascicles
Meniscal displacement relative to tibia
Peripheral meniscal corner tears
Conclusion
: The PPV for MR diagnosis of meniscocapsular separation is low (9% medially,13% laterally)
2. Pelligrini-Stieda Syndrome
Ossification at medial aspect of the knee in either
Medial collateral ligament
Adductor magnus (less common)
Cause is presumably post-traumatic
3. MR criteria for stability of osteochondritis dissecans in knee and ankle. Radiol (1996) 25: 159-163
High-signal-intensity line at interface of fragment and parent bone
Cyst formation
Focal defect in cartilage and subchondral bone
High-signal fluid passing into the lesion
High-signal interface may not indicate instability (granulation tissue vs fluid)
Accuracy of MR for staging OCD lesion improved from 45% to 85% by interpreting high-signal interface as predictor of instability only when accompanied by breach in articular cartilage on T1
4. Posterior shoulder dislocation. Acta Orthop Scand. 1986; 57: 535-536.
In 10/10: Teres minor rupture, posterior capsule rupture, and infraspinatus tear
In 8/10: Lower subscapularis tear
In 10/10: Intact supraspinatus and CH ligament
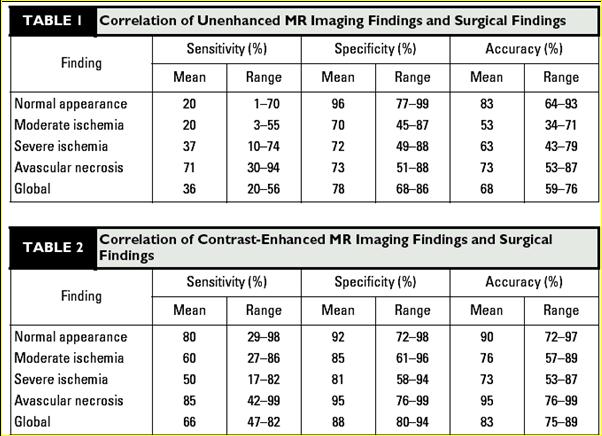
5. Diagnosing AVN in Scaphoid Non-Unions
Conventional radiography and CT: sclerosis of proximal fragment doesn’t correlate
Bone scintigraphy: Very sensitive, non-specific
Surgery: Inspection of punctate bleeding points most accurate
MRI: Low T1, low T2 not reliable
Usefulness of gadolinium-enhanced MR imaging in the evaluation of scaphoid non-unions. AJR 2000; 174: 141-149
30 patients, MRI, surgery, 1-yr follow up
% enhancement of proximal pole was evaluated (>80%, 50-80%, 20-50%, <20%)
6. A medial displaced patella is likely related to previous lateral release.
7. Femoral neck stress fractures. Tensile side fix 100%. Comprressive side, fix 50%, conservative 50%.
8. Subacute muscle denervation causes extracellular water to collect. Chronically becomes fatty.
May 24th Rheum
1. STT joint affected by OA and CPPD
2. Connective tissue disease can have a lot of periarticular appetite.
3. DIPJ central erosions aggressive OA, peripheral gout.
4. If syndesmophytes form later in life, they may form around disc protrusions and be curved.
5. Mimmics for AS include the enteropathic arthropathies; Whipples, intestinal bypass surgery, UC, Crohn's.
6. Toe IPJ; RhA medial, Psoriasis all the way across.
7. The Rh variant of psoriasis has less inflammatory change.
8. RhA of the hips only occurs after a long time.
9. RhA erosions of foot MT heads affect medial 2-4 and lateral 5.
10. RhA if affecting the mid foot is commonest at the talonavicular J
May 17th 2002 Ortho
1. If one of the handles of a bucket handle tear extends into the inner surface of the meniscus it becomes very much like a large parrot beak tear, maybe better described as a Kiwi beak tear (a term coined locally)
Kiwi Parrot
2. DDx for double biceps tendon:
Calcific tendinosis
Body
Longtitudinal split
SLAP 4 proximally
3. Subscap path often starts superiorly
4. Gorham's disease of massive osteolysis is rare. Associated with haemangiomatosis, osteolysis, and disappearing bone. It is sporadic. It violates joints.
5. Haglund's syndrome is the combination of: retrocalcaneal bursitis, achilles tendinopathy, and superficial bursitis. It is related to footwear. Rx: shave off posterior aspect of posterior process of calcaneus. Pump bump is caused by shoes which rub on the heel and produce a superficial bursitis.
 |
ballet pumps court shoe pumps
6. With RhA, marginal erosions are more commonly seen on the tibia
7. The popliteal meniscal ligaments are the lateral meniscal struts. They are superior and inferior. They blend with both the capsule and the popliteus tendon. They help unlock the kne at the beginning of flexion, by pulling on the meniscus.
8. Hawkins sign was first described in the talus.
9. Bicruciate tears suggest dislocation. Plus a colateral makes it likely. All four definite dislocation. can also injure patella tendon.
10. The arcuate complex is made up of the fabelofibula ligament, the arcuate ligament, and the popliteal fibula ligament. All 3 attach to the fibula styloid.
11. A meniscal flounce does not imply a tear. A double flounce makes a tear more likely. Often seen in arthrograms due to applied stress. They possibly imply that a tear is unstable or complete (inside edge to periphery)
12. Congenital absence of the ACL is rare. It is possibly resorption of ACL post tear, but this is also rare. May be a smaller tibial eminence between spines if congenitally absent.
13. Tennis shoes tend to grow pseudomonas so beware of this with penetrating tennis shoe injuries.
14. Meniscal ossicles are rare. They are usually medial. They are seen in tigers and possibly reptiles.
15. When assessing for arthrofibrosis it is useful to look at the T1 images side by side with the FS.
16. Adhesive capsulitis shows thickening of the axillary recess >4mm and the rotator interval, with enhancement. May also have calcification of the inferior recess. A similar appearance may be seen on the undersurface of the medial scapular following luxatio erecta.
May 15th 2002 Navy
1. Two receptors on cartilage, PTH and Indian hedgehog IHH. In Maffucci's the PTH receptor is abnormal and the IHH is unopposed. It is due to a spontaneous mutation.
2. Parasites that calcify.
Trichonosis
Schistosomiasis
Echinococcus
Dracunculus medinensis, Becomes beaded due to movement, possible tumour related.
Armillifer armillatus
Loa loa, Filiaria
Cystercerci, Pork Tape worm
3. Meniscal cysts are slightly more common medially. They may be intra or peri meniscal. They occ. cause bone erosion.
4. Following patella tendon grafting for ACL repair cystic/mucinous degeneration may occur.
5. Femoral neck erosion:
Synovial osteochondromatosis, very rarely associated with synovial chondrosarcoma
PVNS
Gout, rare in hip
Amyloid
TB
6. Osteoid osteoma likely often starts subperiosteal and appears to become intracortical with new bone formation. When intraarticular sclerosis may appear remote from nidus.
7. Pagets only rarely affects fibula, clavicle and rib.
8. SAPHO Hyperostosis of clavicle, more commonly medial. Sternocostoclavicular hyperostosis is a subgroup of this. Can also affect chest wall. Children may get massive clavicle enlargement. Children more commonly titled CRMO and have chronic symmetric osteitis, often involving metaphyses as well. May occ. grow P.acne, but possibly a contaminant. Always consider SAPHO if osteitis pubis or osteitis condensans ilii is unilateral.
9. Engelman Camurati is symmetric mid diaphyseal sclerosis, Ribbings is similar, but asymmetric. Both are idiopathic intramedullary sclerosis. Both AD. Erdheim Chester a lipid storage disease looks more like multiple infarcts, with more heterogenous look. These diaphyseal conditions spare the epiphyses. Worth's and Van Buchan are smooth endosteal hyperostosis.
10. Fibrous dysplasia looks very heterogenous on MRI.
11. Ivory vertebrae - lymphoma.
12. Cysic angiomatosis can have a variable appearance, varying from sclerotic lesions mimicing prostate mets, to serpentine lytic lesions involving bone and soft tissue.
13. LSMFT does not contain fat, to distinguish from involuting lipoma.
14. With bone in bone due to growth arrest/recovery, the inner fat is usually brighter than the outer when seen in an epiphysis.
15. Intraosseous air implies a benign lesion. Seen at SIJ, vertebrae and glenoid. Lymphangiomatosis of bone may contain gas.
16. Parsonage Turner is likely a post viral neuropathic myositis, most commonly affecting suprascapular and axillary nerves. Entrapment neuropathy, suprascapular nerve - supraspinatus/ infraspinatus, axillary nerve in quadrilateral space - deltoid and teres minor. Other myositis causes includes poly myositis, dermatomyositis, and inclusion body myositis.